Catalysts#
Navigating the Uncharted: Risk Characterization in Living Kidney Donation#
In the expanding narrative of living kidney donation, the demographic shift toward older donors has introduced new complexities to the ethical landscape of informed consent. With the enterprise of living kidney donation represented by the Organ Procurement and Transplantation Network (OPTN), and the digital twin control population modeled using the National Health and Nutrition Examination Survey (NHANES), we are presented with a unique intersection of innovation and obligation. The digital twin functions as a sentinel, an agentic input layer designed to guide prospective donors through the labyrinth of risk, grounding decisions in quantifiable realities rather than anecdotal fears.
A poignant example of this demographic shift occurred in May 2019, when an 84-year-old man became one of the oldest living kidney donors in the United States. His story exemplifies the courage and complexity inherent in advanced-age donation. The consent processes for such candidates often rely on extrapolated data from younger cohorts, typically with a median age of 40 years. This reliance highlights a critical gap in the evidence base: the systematic characterization of risks for older donors remains insufficient. The absence of robust metrics, such as frailty—a condition strongly associated with increased perioperative complications—exacerbates this challenge, leaving critical questions unanswered for donors who deserve clarity.
Perioperative mortality among living donors is rare, with a 90-day risk estimated at 3 per 10,000. However, not all causes of death within this period can be attributed to the nephrectomy itself. Consider the inclusion of homicide within these statistics. It would be erroneous to enumerate such events as perioperative risks, yet their presence underscores the necessity of precise controls. The digital twin—a statistical construct built from NHANES and registry linkages to the National Death Index—provides an indispensable framework for contextualizing these risks. It allows us to distinguish nephrectomy-attributable risks from broader societal and demographic variables, thereby refining the narrative for prospective donors.
For young, healthy donors under 40 who self-report “Very Good or Excellent” health, the nephrectomy-attributable risk is approximately 0.9 per 10,000—a figure significantly lower than the generalized risks often cited during consent. This precision is particularly crucial as the donor population ages. Among nondonors over 50, the 90-day mortality risk aligns closely with their donating counterparts, suggesting that nephrectomy-attributable risks may diminish with age. Yet, the scarcity of data for older cohorts limits definitive conclusions. This underscores the urgent need for comprehensive data collection and targeted research to optimize outcomes for this evolving demographic.
The implications of these findings extend beyond risk estimation. They demand a rethinking of how informed consent is structured, particularly for older candidates. Consent processes must evolve from static presentations of generalized risks to dynamic, individualized narratives that integrate the donor’s unique health profile with contextualized data from their digital twin. By leveraging tools like cumulative incidence estimates derived from Cox regression models, we can present a more accurate, transparent picture to potential donors. This approach not only respects their autonomy but also fortifies their agency in making life-altering decisions.
The story of advanced-age donation is emblematic of the broader challenges facing the enterprise of living kidney donation. As we stand on the cusp of demographic transformation, the enterprise must adapt, guided by the dual beacons of innovation and ethical rigor. The digital twin, as a control population, offers a pathway to clarity, transforming abstract data into actionable insights. Yet, the journey is far from complete. Frailty, a critical metric, remains largely uncaptured in existing databases, leaving a chasm that must be bridged to ensure that the narrative of living kidney donation remains both scientifically grounded and ethically sound.
In the grand tapestry of healthcare, living kidney donation represents a luminous thread, intertwining altruism with medical advancement. But even the brightest threads can fray without vigilance. By systematically addressing the gaps in data and refining our tools for risk characterization, we can preserve the integrity of this enterprise, ensuring that each donor’s decision is anchored in truth and trust.
Show code cell source Hide code cell source
import numpy as np
import matplotlib.pyplot as plt
import networkx as nx
# Define the neural network structure; modified to align with "Aprés Moi, Le Déluge" (i.e. Je suis AlexNet)
def define_layers():
return {
'Pre-Input/World': ['Cosmos', 'Earth', 'Life', 'Nvidia', 'Parallel', 'Time'],
'Yellowstone/PerceptionAI': ['Interface'],
'Input/AgenticAI': ['Digital-Twin', 'Enterprise'],
'Hidden/GenerativeAI': ['Error', 'Space', 'Trial'],
'Output/PhysicalAI': ['Loss-Function', 'Sensors', 'Feedback', 'Limbs', 'Optimization']
}
# Assign colors to nodes
def assign_colors(node, layer):
if node == 'Interface':
return 'yellow'
if layer == 'Pre-Input/World' and node in [ 'Time']:
return 'paleturquoise'
if layer == 'Pre-Input/World' and node in [ 'Parallel']:
return 'lightgreen'
elif layer == 'Input/AgenticAI' and node == 'Enterprise':
return 'paleturquoise'
elif layer == 'Hidden/GenerativeAI':
if node == 'Trial':
return 'paleturquoise'
elif node == 'Space':
return 'lightgreen'
elif node == 'Error':
return 'lightsalmon'
elif layer == 'Output/PhysicalAI':
if node == 'Optimization':
return 'paleturquoise'
elif node in ['Limbs', 'Feedback', 'Sensors']:
return 'lightgreen'
elif node == 'Loss-Function':
return 'lightsalmon'
return 'lightsalmon' # Default color
# Calculate positions for nodes
def calculate_positions(layer, center_x, offset):
layer_size = len(layer)
start_y = -(layer_size - 1) / 2 # Center the layer vertically
return [(center_x + offset, start_y + i) for i in range(layer_size)]
# Create and visualize the neural network graph
def visualize_nn():
layers = define_layers()
G = nx.DiGraph()
pos = {}
node_colors = []
center_x = 0 # Align nodes horizontally
# Add nodes and assign positions
for i, (layer_name, nodes) in enumerate(layers.items()):
y_positions = calculate_positions(nodes, center_x, offset=-len(layers) + i + 1)
for node, position in zip(nodes, y_positions):
G.add_node(node, layer=layer_name)
pos[node] = position
node_colors.append(assign_colors(node, layer_name))
# Add edges (without weights)
for layer_pair in [
('Pre-Input/World', 'Yellowstone/PerceptionAI'), ('Yellowstone/PerceptionAI', 'Input/AgenticAI'), ('Input/AgenticAI', 'Hidden/GenerativeAI'), ('Hidden/GenerativeAI', 'Output/PhysicalAI')
]:
source_layer, target_layer = layer_pair
for source in layers[source_layer]:
for target in layers[target_layer]:
G.add_edge(source, target)
# Draw the graph
plt.figure(figsize=(12, 8))
nx.draw(
G, pos, with_labels=True, node_color=node_colors, edge_color='gray',
node_size=3000, font_size=10, connectionstyle="arc3,rad=0.1"
)
plt.title("Archimedes: Staying Aloat & Navigating the Donor Evaluation Process", fontsize=15)
plt.show()
# Run the visualization
visualize_nn()
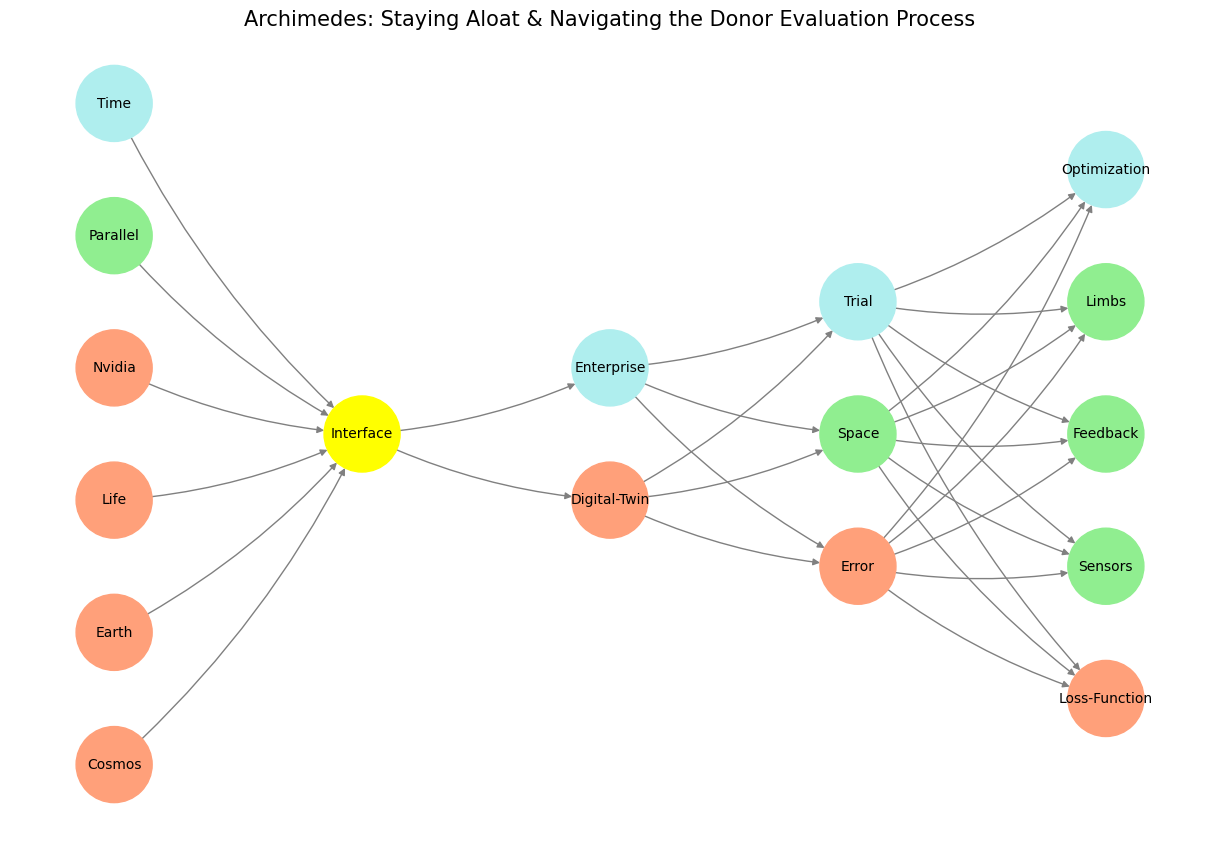

Fig. 4 In our scenario, living kidney donation is the enterprise (OPTN) and the digital twin is the control population (NHANES). When among the perioperative deaths (within 90 days of nephrectomy) we have some listed as homicide, it would be an error to enumerate those as “perioperative risk.” This is the purpose of the digital twin in our agentic (input) layer that should guide a prospective donor. There’s a delicate agency problem here that makes for a good case-study.#

