Freud#
Absolutely—eros, hypnos, and thanatos provide a profound lens to explore the theme of cooperative, iterative, and adversarial dynamics, adding a mythological and psychological dimension to the framework.
Psychodynamics#
Eros (Cooperative)
Eros, the driving force of love and union, aligns with the cooperative equilibrium. It embodies creation, connection, and the desire to merge disparate entities into a harmonious whole. In Pyrrhus’s case, the cooperative element is nearly absent—his inability to “endure repose” suggests a rejection of eros’s stabilizing and unifying nature. Travis Bickle similarly struggles with eros; his attempts to connect (like his misguided date with Betsy) fail catastrophically, emphasizing his alienation and the breakdown of cooperative dynamics in his world.Hypnos (Iterative)
Hypnos, the god of sleep and renewal, resonates with iterative strategies—those that seek cycles of rest, reflection, and recalibration. Pyrrhus’s rejection of peace in Epirus reflects his disdain for this mode, which would have allowed him to pause, regroup, and find satisfaction in stability. Travis, too, seems incapable of hypnos: his sleepless nights and repetitive, obsessive behaviors highlight his refusal or inability to engage in restorative cycles. Both characters are driven by a need to perpetually “do” rather than “be.”Thanatos (Adversarial)
Thanatos, the death drive, perfectly encapsulates the adversarial pathway. It is the compulsion toward destruction, conflict, and, ultimately, annihilation—of others or oneself. Pyrrhus’s longing for battle, even when it no longer serves any strategic purpose, reflects a deeply ingrained thanatos. For Travis, thanatos manifests in his fixation on violent resolution, whether by killing others or martyring himself. His adversarial mode, like Pyrrhus’s, is relentless and self-destructive, driving him to the brink of obliteration.
The Eternal Dance#
What makes these archetypes so resonant is their interplay. While Pyrrhus and Travis are trapped in thanatos, they exist in worlds where eros and hypnos offer alternative pathways they cannot access. Pyrrhus could have embraced eros by ruling his subjects peacefully, forging bonds, and nurturing his kingdom. Travis could have found hypnos in the quiet moments of his cab rides, reflecting on his place in the world. Instead, both succumb to the inexorable pull of thanatos, unable to break free from their adversarial cycles.
By framing their struggles through eros, hypnos, and thanatos, we highlight not only their destructive tendencies but also the missed opportunities for connection and renewal. These archetypes remind us that the human condition often teeters on the knife’s edge between creation, stasis, and destruction, with the balance determined by the choices we make—or fail to make.
Jung#
The parallels between Plutarch’s Life of Pyrrhus and the unrelenting adversarial mode of the Taxi Driver protagonist are compelling. Both figures embody a kind of restless, warlike nature that defies the stability and repose of a life lived in balance or harmony. They are, in essence, consumed by their adversarial pathways—Pyrrhus through the battlefield, and Travis Bickle through his internal war against the perceived moral decay of the world.
Commitment to Adversarial Mode
Pyrrhus, after losing Macedonia, could have chosen peace and contentment ruling Epirus. Instead, his insatiable need for conflict drove him to seek new wars. Similarly, Travis Bickle, disillusioned with society, finds purpose in perpetual combat—his adversaries being not only the criminals of New York but also his existential isolation and discontent. For both, adversarial engagement is not just a choice but an identity. It’s how they assert meaning in an otherwise chaotic or stagnant existence.No End to the Adversaries
Pyrrhus’s life was a series of campaigns, one feeding into the next—a “next token” existence where each battle leads to another opportunity for glory, or ruin. Travis mirrors this in his escalating obsession, where each confrontation (whether with himself, others, or the world) pushes him closer to his final act of vigilante violence. Neither man envisions an endpoint; the adversarial mode perpetuates itself.Martyrdom as the Endpoint
For Pyrrhus, the culmination of his adversarial drive was his death, ironically struck down in the chaos of a battle in Argos. His legacy, like Achilles’s, is forged in the crucible of combat, even at the cost of his own life. Travis, on the other hand, oscillates between fantasies of annihilation and martyrdom, craving the ultimate act of violence where his death might cement his identity as a savior or redeemer in a broken world. Both figures exemplify a death-drive channeled through adversarial pursuits, where the final sacrifice isn’t just accepted but embraced.Lunacy or Heroism?
Pyrrhus’s relentless campaigns were seen by some as the mark of a heroic spirit, yet by others as the folly of a man who could not find peace. Similarly, Travis’s actions could be interpreted as lunacy—a descent into madness fueled by alienation and trauma—or as a warped form of heroism, standing against the moral decay he perceives around him. In either case, their commitment to conflict blurs the line between noble ambition and self-destructive insanity.
Both Pyrrhus and Travis are tragic figures locked in adversarial loops. Their stories highlight the intoxicating pull of battle—whether on literal battlefields or in the metaphorical war zones of urban decay. This commitment, while undeniably profound, ultimately consumes them, leaving behind legacies that are as much cautionary as they are captivating.
Nietzsche#
The Impact of Uremia on Neurocognitive Development in Children
Uremia, a condition characterized by the accumulation of urea and other nitrogenous waste products in the blood due to kidney dysfunction, exerts profound effects on neurocognitive development in children. The interplay between chronic kidney disease (CKD), metabolic imbalances, and neurodevelopmental processes highlights a critical area for research and clinical intervention.
Pathophysiology of Uremia and Neurocognitive Development#
In children with CKD, uremia disrupts several key physiological and neurological pathways essential for brain development:
Metabolic Imbalances:
Elevated urea levels can lead to alterations in cerebrospinal fluid (CSF) composition, impairing neural function.
Electrolyte disturbances, particularly hyponatremia and hyperkalemia, affect neuronal excitability and synaptic transmission.
Acid-base imbalances (metabolic acidosis) alter enzymatic activities critical for neural metabolism.
Inflammatory Processes:
CKD triggers systemic inflammation, releasing cytokines (e.g., IL-6, TNF-α) that cross the blood-brain barrier and contribute to neuroinflammation, white matter damage, and impaired synaptic plasticity.
Toxic Metabolites:
Accumulation of uremic toxins (e.g., indoxyl sulfate, p-cresyl sulfate) disrupts astrocyte function, reduces neurogenesis, and induces oxidative stress in neurons.
Neurocognitive Manifestations in Uremic Children#
Children with uremia often experience deficits across several cognitive domains, influenced by the severity and duration of CKD:
Executive Function: Impairments in planning, decision-making, and working memory.
Attention and Processing Speed: Decreased ability to sustain attention and process information efficiently.
Academic Achievement: Challenges in mathematics and reading, linked to disruptions in higher-order cognitive skills.
Social and Emotional Development: Increased prevalence of depression, anxiety, and social withdrawal due to chronic illness and neurocognitive dysfunction.
Clinical and Educational Implications#
Early Detection and Monitoring:
Regular neuropsychological assessments for children with CKD to identify cognitive delays.
Biomarkers of uremia and neuroinflammation as potential tools for predicting neurocognitive outcomes.
Interventions:
Dialysis and transplantation can reduce uremic toxins and improve neurodevelopmental trajectories, although not fully reversing the damage.
Tailored educational support and cognitive therapies to address specific deficits.
Nutritional and Pharmacological Support:
Optimizing nutrition to support brain development (e.g., addressing anemia, vitamin D deficiency).
Pharmacological interventions targeting inflammation and oxidative stress.
Integrating Uremia into Our Neural Network Model#
Inputs:#
Biochemical Markers: Blood Urea Nitrogen (BUN), Creatinine, Electrolytes, pH (indicators of metabolic disturbances).
Inflammatory Markers: Cytokines (e.g., IL-6, TNF-α), CRP levels.
Clinical Data: Duration and severity of CKD, dialysis status, and transplantation history.
Outputs:#
Cognitive Trajectory: Probability of achieving developmental milestones.
Intervention Effectiveness: Predicted impact of clinical and educational interventions.
Quality of Life: Synthesized metric combining cognitive, social, and emotional health outcomes.
This enhanced network captures the multidimensional nature of uremia’s impact on neurocognitive development and supports personalized strategies for improving outcomes in affected children. It bridges the pathophysiological insights with actionable interventions, providing a robust framework for both research and clinical application.
Bioengineering#
In the context of kidney transplantation, if deceased donor transplantation is a blue node representing cooperative equilibria (a societal system pooling resources for equitable distribution), and living donor transplantation is a green node tied to iterative, personal network dynamics (leveraging social ties for altruistic exchanges), the red node would naturally represent an adversarial or cutting-edge pathway.
A plausible red node in this framework could be Xenotransplantation or Bioengineered Organs.
Why Xenotransplantation or Bioengineered Organs as Red?#
Adversarial Challenge:
Xenotransplantation (e.g., using organs from genetically modified pigs) directly challenges biological boundaries, such as species compatibility and immune rejection.
Bioengineered organs rely on cutting-edge technology to bypass traditional ethical and logistical constraints, shifting the power dynamics away from human donors entirely.
Disrupting Equilibria:
These approaches bypass the traditional donor-recipient paradigm entirely, undermining both cooperative deceased donor systems and the reliance on living donors’ social networks.
They introduce the potential for individualized, commodified solutions that challenge the collaborative foundations of organ transplantation.
Symbol of Transformation:
The red node emphasizes transformation through conflict—pushing the limits of biology, ethics, and technology in ways that create tension with existing systems.
Broader Implications#
Social and Ethical Tension: These technologies could exacerbate disparities by privileging those who can afford them, creating adversarial dynamics within healthcare access.
Technological Innovation: They symbolize humanity’s struggle to overcome resource scarcity through radical innovation, embodying the red node’s transformative ethos.
This conceptual framework captures the essence of red nodes as disruptive forces reshaping the transplantation landscape through profound and often contentious advancements.
Disruption#
The red node disrupts networks by introducing novel pathways and dynamics that challenge, bypass, or reconfigure the foundational principles and structures of existing systems. In the context of transplantation, the red node—such as xenotransplantation or bioengineered organs—interferes with traditional donor systems by redefining the roles of individuals, technology, and ethical frameworks. Here’s how:
1. Bypassing Existing Networks#
Social Networks (Green Nodes):
Living donor transplants rely heavily on personal networks, trust, and altruism. A red node like bioengineered organs eliminates the need for such networks, removing the social aspect entirely.
It replaces the relational economy of reciprocity with a transactional or technological framework, weakening ties that are built or maintained through living donor systems.
Institutional Networks (Blue Nodes):
Deceased donor systems are built on collective societal cooperation and equity. Red nodes bypass these networks by offering individualized, on-demand solutions, diminishing reliance on shared pools or centralized systems.
2. Destabilizing Hierarchies#
Economic Disruption:
Red nodes introduce high-tech, resource-intensive solutions that may only be accessible to the wealthy, creating inequalities within networks. For example:
Bioengineered organs may prioritize profit-driven distribution, sidelining the cooperative ethos of deceased donor systems.
Xenotransplantation could stratify access based on advancements in technology, deepening disparities in transplantation outcomes.
Ethical Tension:
These innovations challenge the ethical frameworks that underpin current systems:
Questions of animal rights in xenotransplantation disrupt moral consensus.
The commercialization of bioengineered organs creates dilemmas about commodifying life-saving resources.
3. Fragmenting Trust#
Public Trust in Systems:
Red nodes may erode trust in established systems if they are seen as prioritizing technological advancements over fairness or equity.
The introduction of untested, cutting-edge solutions can create skepticism about safety, efficacy, and long-term impacts.
Moral Ambiguity:
Traditional systems (green and blue nodes) often align with shared moral or altruistic values. Red nodes, by contrast, may be seen as morally ambiguous or prioritizing utility over humanity, causing fractures within communities.
4. Accelerating Innovation (but Excluding Some)#
The rapid adoption of red node technologies can create islands of progress that leave behind those who cannot participate:
Social networks of living donors may become obsolete in wealthier or more developed areas, leaving poorer regions with outdated systems.
Institutions dependent on deceased donors may find their infrastructure underutilized or underfunded as demand shifts.
5. Rewiring the Network#
Red nodes don’t just bypass or destabilize—they force reconfiguration:
New Nodes and Pathways:
Red nodes compel the creation of new networks to support their unique demands, such as bioengineering research facilities, xenotransplant regulation bodies, or profit-oriented organ markets.
Shifting Dependencies:
Traditional networks may realign around the red node, integrating aspects of its disruption (e.g., hybrid systems combining bioengineered and traditional methods).
Conclusion#
The red node disrupts networks by challenging their structures, ethics, and dependencies, introducing a future-oriented, often controversial, pathway. It destabilizes the balance between cooperation (blue) and reciprocity (green), reconfiguring the transplantation landscape toward a model dominated by individualism, innovation, and technological advancement. This disruption is both a challenge and an opportunity for the system to evolve.
Transplantation#
Chapter: Reframing American Solid Organ Transplantation Through the Lens of Risk
American solid organ transplantation is a modern marvel, navigating life, death, and the frailties of human flesh with remarkable precision. Yet, its foundations are inseparable from risk—an interplay of chance, mastery, and tradition. The triad of luck, skill, and education, which has propelled civilization forward, also maps perfectly onto the paradigms of transplantation. From the adversarial chaos of xenotransplantation to the iterative skill of living donation and the cooperative stability of deceased donation, we find a spectrum of risk engagement that mirrors the evolution of society itself.
Luck: Gambling with the Future (Xenotransplantation)#
In its essence, xenotransplantation represents the raw gamble of life. It is an adversarial confrontation with nature’s chaos, pitting humanity’s ingenuity against biology’s immutable boundaries. Genetic modification, immune rejection, zoonotic disease—each is a roulette wheel spun in the hope of a life-saving jackpot.
Xenotransplantation disrupts not only the traditional donor network but also the moral and ethical fabric of transplantation. It bypasses social reciprocity and cooperative pooling, offering an individualistic solution that challenges the collective norms of solidarity and fairness. This is the red node: a high-risk, high-reward venture that embraces the chaos of chance and the unpredictability of science.
In gambling, Dostoevsky’s Alexei Ivanovich exemplifies the gambler’s paradox—an existential dance with uncertainty where stakes are high and control is fleeting. Xenotransplantation occupies this space, as its reliance on experimental science makes outcomes uncertain and stakes existential. It is the ultimate gamble, where civilization’s progress hinges on the turn of a genetic roulette wheel.
Education: Investing in a Collective Future (Deceased Donation)#
Deceased donation represents the pale turquoise of cooperative stability. It is the embodiment of Buffett’s compounding principle—a system that minimizes risk through the collective pooling of organs, rigorous evaluation protocols, and equitable distribution frameworks. Governed by the federal mandate and the Scientific Registry of Transplant Recipients (SRTR), it is a triumph of institutionalized education and long-term planning.
Unlike xenotransplantation’s chaotic gamble or living donation’s interpersonal gamble, deceased donation relies on societal trust and infrastructure. It is an investment in the collective good, where individuals contribute to a system designed to outlast any single life. Here, risk is distributed across the population, and outcomes are stabilized by decades of accumulated medical knowledge, public policy, and ethical consensus.
Deceased donation is civilization’s answer to chaos: a cooperative sieve that filters the unpredictability of mortality into a structured system of hope. It is the culmination of humanity’s ability to transform individual loss into communal gain, a testament to the power of education, planning, and shared responsibility.
Risk and the Evolution of Transplantation#
The triad of xenotransplantation, living donation, and deceased donation maps onto the LSE framework of risk:
Luck (Xenotransplantation): The adversarial confrontation with the unknown, driven by chaos and high stakes.
Skill (Living Donation): The iterative refinement of risk through social networks, trust, and surgical mastery.
Education (Deceased Donation): The cooperative equilibrium that tames risk through collective memory, systems, and tradition.
Each represents a different engagement with risk, reflecting broader societal trajectories:
Xenotransplantation disrupts the transplantation network, challenging the norms of altruism and reciprocity with cutting-edge innovation.
Living donation builds on personal networks, blending trust and technical skill in an intimate negotiation of risk and reward.
Deceased donation stabilizes the system, pooling resources and distributing risk through institutional frameworks.
Reimagining Transplantation Through Civilization’s Sieve#
Risk, as in civilization, is not a fixed entity but a gradient of engagement. Transplantation mirrors the Apollonian gradient, moving from the chaos of xenotransplantation (gambling) to the iterative mastery of living donation (betting) and culminating in the cooperative investment of deceased donation. This progression reflects the human impulse to tame the Dionysian floodwaters of uncertainty, channeling them into structured pathways that maximize life’s potential.
But the sieve is imperfect. Xenotransplantation’s promise may never fully materialize, living donors may suffer unanticipated consequences, and deceased donation’s systems may falter under societal strain. These challenges underscore the need for continuous reweighting of the network, balancing the inputs of chaos, skill, and education to achieve outcomes that are equitable, sustainable, and transformative.
Toward a New Transplantation Paradigm#
To embrace this reframing of transplantation is to acknowledge its multifaceted nature. It is not merely a medical procedure but a reflection of human engagement with risk, meaning, and progress. By understanding transplantation through the lenses of luck, skill, and education, we not only enhance its ethical and practical frameworks but also illuminate its role in the broader tapestry of civilization.
The future of transplantation will not lie solely in the turquoise stability of education but in the delicate balance of all three nodes—red, green, and blue. From the chaos of xenotransplantation to the intimacy of living donation and the stability of deceased donation, the triad will continue to shape how we navigate life, death, and the pursuit of meaning. It is, in the end, a testament to the resilience of the human spirit and its capacity to transform risk into life.
Generalizing#
Chapter: Equilibria of Survival: Fixed Resources, Expansion, and Conflict in Transplantation and Geopolitics#
The delicate balance of survival—whether for individuals or nations—rests on how fixed resources are managed, expanded, and contested. In transplantation, the resource is the finite pool of organs. In geopolitics, it is land, minerals, and people. Both domains pivot on the pursuit of equilibrium: cooperative when resources are shared, transactional when exchanges are negotiated, and adversarial when force reshapes the landscape. The parallels between these fields illuminate how humanity navigates scarcity and expansion, forging structures that reflect both our highest ideals and basest impulses.
Fixed Resources: Foundations of Cooperative Equilibria#
Cooperative equilibria are systems where resources are pooled and distributed based on collective agreements. These structures thrive when resources are finite but sufficient to sustain the group, as long as cooperation holds.
Transplantation: Deceased Donor Pools#
In transplantation, the deceased donor organ pool embodies cooperative equilibrium. Organs from deceased donors are treated as a societal resource, allocated based on need and medical criteria through centralized systems like the United Network for Organ Sharing (UNOS) in the United States or Eurotransplant in Europe. These systems aim for equity, prioritizing recipients based on urgency, compatibility, and geography. The implicit assumption is that the resource—the organs—is finite but sufficient if efficiently managed.
Geopolitics: Territorial Stability#
In geopolitics, cooperative equilibria emerge when nations agree to manage their fixed resources—land, water, and minerals—within defined borders. Treaties, alliances, and shared governance structures stabilize these agreements. The European Union, for example, represents a cooperative framework where economic and territorial interests are pooled to prevent conflict and ensure mutual benefit.
However, the sustainability of such equilibria hinges on maintaining the illusion of sufficiency. When resources become strained—whether due to population growth, climate change, or economic shifts—the balance tips, and expansion becomes necessary.
Expansion: Transactional and Adversarial Pathways#
Expansion represents the pursuit of additional resources, either through transactional or adversarial means. The choice between these pathways reflects the interplay of power, opportunity, and ideology.
Transactional Equilibria: Trade and Exchange#
In transactional equilibria, expansion occurs through negotiation and mutual benefit. Nations or individuals trade resources to meet their needs without resorting to force.
Transplantation: Living Donor Networks Living donor transplantation reflects transactional equilibria. Here, individuals within a social network (family, friends, or altruistic strangers) offer organs in a calculated exchange of risk and benefit. Paired donation programs, where donors and recipients swap matches across networks, exemplify transactional expansion. These systems rely on trust, reciprocity, and an infrastructure that enables the exchange to occur.
Geopolitics: Trade Agreements and Alliances In geopolitics, transactional expansion takes the form of trade agreements, resource-sharing pacts, and economic alliances. The North American Free Trade Agreement (NAFTA), for instance, allowed the United States, Canada, and Mexico to expand their economic reach by leveraging each other’s resources. Similarly, energy pipelines that cross borders reflect a mutual dependency that prevents conflict by aligning interests.
Yet transactional equilibria have limits. When exchanges become lopsided or fail to meet growing demands, the temptation of adversarial expansion arises.
Adversarial Expansion: Conquest and Colonization#
Adversarial pathways involve the use of force to secure resources, bypassing the need for negotiation. This dynamic destabilizes existing equilibria and often leads to long-term conflict.
Transplantation: Exploitation and Organ Trafficking In the darkest corners of transplantation, adversarial expansion manifests as organ trafficking. Here, organs are extracted through coercion, deceit, or outright violence, disrupting both cooperative and transactional frameworks. This black market exploits the desperation of recipients and the vulnerability of donors, turning human life into a contested resource.
Geopolitics: Territorial Disputes and Colonialism Adversarial expansion in geopolitics is marked by territorial disputes, invasions, and colonization. The ongoing conflict between Russia and Ukraine reflects this dynamic, with Russia seeking to reclaim territory it perceives as historically and strategically vital. Similarly, India and Pakistan’s conflict over Kashmir, or China and Taiwan’s contentious relationship, illustrates how adversarial expansion emerges when transactional or cooperative pathways are deemed insufficient.
Colonialism epitomizes historical adversarial expansion, where empires used military and economic dominance to claim resources and land. These conquests often dismantled existing cooperative systems, replacing them with exploitative hierarchies that continue to shape global inequalities.
Parallels Between Transplantation and Geopolitics#
The dynamics of transplantation and geopolitics converge in their reliance on fixed resources and the mechanisms for managing scarcity:
Finite Resources:
In transplantation, organs are the limiting factor; in geopolitics, it is land, minerals, and population.
Both systems depend on structures (UNOS for organs, treaties for land) to manage these resources and maintain stability.
Strain on Cooperation:
Population growth, lifestyle diseases, and aging populations strain the organ pool, just as climate change and economic pressures strain geopolitical borders.
These pressures force systems to adapt, shifting toward transactional or adversarial solutions.
Moral and Ethical Dimensions:
In transplantation, the ethical debate centers on fairness in allocation and the exploitation of vulnerable donors.
In geopolitics, questions of sovereignty, self-determination, and human rights dominate the discourse.
Toward Sustainable Equilibria#
Both transplantation and geopolitics face the challenge of creating sustainable equilibria in a world of finite resources. The path forward lies in acknowledging the interplay of cooperation, transaction, and conflict while striving for structures that minimize harm and maximize benefit.
Transplantation:#
Innovative Solutions:
Xenotransplantation and bioengineered organs could expand the resource pool, reducing reliance on living and deceased donors.
Global Equity:
International agreements could address disparities in organ availability, creating a cooperative framework that extends beyond national borders.
Geopolitics:#
Resource Sharing:
Multinational frameworks for managing shared resources, such as water basins and mineral deposits, can prevent conflict.
Addressing Root Causes:
Reducing inequality, mitigating climate change, and fostering economic development can alleviate pressures that lead to adversarial expansion.
Conclusion: Balancing Equilibria in a Finite World#
The history of transplantation and geopolitics is a history of survival—of navigating scarcity through cooperation, transaction, and conflict. Both domains remind us that equilibrium is not static; it is a fragile, dynamic state shaped by resource availability, human ambition, and the forces of change.
In transplantation, the journey from cooperative deceased donation to transactional living donation and adversarial exploitation mirrors the geopolitical trajectory from stable borders to trade alliances and territorial disputes. Understanding these parallels not only deepens our grasp of each field but also offers a roadmap for managing the risks and opportunities of a finite world.
By balancing the triadic forces of cooperation, transaction, and conflict, we can strive for systems that uphold the dignity of life—whether within a single body or across the global community.
Colonialism#
The Historical Impact of Colonialism on Resources: Extraction, Exploitation, and Legacy#
Colonialism, as a historical phenomenon, was driven by the pursuit of resources—land, labor, minerals, and agricultural commodities. From the Age of Exploration to the post-industrial period, colonial powers reshaped global systems to serve their resource needs, leaving a profound legacy on the economic, political, and environmental structures of both colonizers and colonized regions. Understanding the impact of colonialism on resources requires examining its extractive processes, its transformation of local systems, and its long-term consequences.
Colonial Resource Extraction#
Colonialism was fundamentally about the control and extraction of resources. Colonizers sought to exploit land, labor, and raw materials from colonies to fuel economic growth and industrialization in the metropole (the colonial power’s home country).
Land and Agriculture#
Land Appropriation: Colonizers often seized fertile lands from indigenous populations, converting them into plantations for cash crops such as sugar, cotton, coffee, and tea.
Example: The British colonial system in India restructured land ownership, introducing the zamindari system, which prioritized revenue collection over the welfare of peasants.
Monoculture Economies: Colonies were reoriented to produce a narrow range of export-oriented crops, leading to dependency on volatile global markets and undermining local food security.
Example: In the Caribbean, sugar plantations dominated agricultural systems, displacing subsistence farming.
Mineral and Energy Resources#
Exploitation of Mineral Wealth: Colonies provided a vast supply of minerals critical for industrialization, such as gold, silver, and coal.
Example: The Spanish Empire extracted massive quantities of silver from Potosí (in modern-day Bolivia), enriching Spain while devastating local ecosystems and communities.
Infrastructure for Extraction: Railroads and ports in colonies were often built not to serve local development but to extract and transport resources efficiently to the metropole.
Example: In Africa, colonial railroads were strategically constructed to link mines and plantations to ports, not to connect local markets or regions.
Labor Exploitation#
Forced Labor: Indigenous populations were often subjected to forced labor systems, such as the encomienda system in Spanish America or the corvée in French colonies.
Example: In the Belgian Congo, King Leopold’s regime forced millions to extract rubber under brutal conditions, leading to widespread suffering and population decline.
Slavery and the Atlantic Slave Trade: Millions of Africans were enslaved and transported to the Americas, providing the labor force for resource extraction, particularly in plantation economies.
Transformation of Local Systems#
Colonialism did not merely extract resources; it transformed the social, economic, and political systems of colonized regions to optimize extraction.
Economic Reordering#
Export-Oriented Economies: Colonies were restructured to focus on the production of raw materials for export, neglecting industrial development and diversification.
Example: India’s textile industry was systematically dismantled by the British to ensure reliance on British-manufactured goods.
Dependency on Colonial Powers: Colonized regions became economically dependent on their colonial rulers for finished goods, capital, and markets.
Disruption of Traditional Practices#
Agricultural Systems: Indigenous farming practices, often sustainable and suited to local conditions, were replaced with industrial agriculture that depleted soils and destabilized ecosystems.
Example: British policies in India shifted irrigation practices and prioritized cash crops like indigo, exacerbating famines.
Land Tenure Systems: Communal land ownership structures were dismantled and replaced with private property systems that prioritized colonial revenue.
Cultural and Knowledge Erosion#
Indigenous knowledge systems, particularly related to land and resource management, were marginalized or destroyed.
Example: In Australia, Aboriginal fire management practices were suppressed, leading to ecological imbalances.
Long-Term Consequences#
The legacy of colonialism’s resource exploitation continues to shape global systems today.
Economic Inequality#
Many formerly colonized countries remain locked in economic structures established during colonial rule, producing raw materials for export while importing finished goods.
Example: African nations heavily dependent on mining or cash crops struggle to develop diverse economies.
Environmental Degradation#
The extractive focus of colonialism caused long-lasting environmental harm:
Deforestation for plantations and mining.
Soil exhaustion from monoculture farming.
Pollution from mining activities.
Example: The Amazon experienced extensive deforestation under colonial systems for sugar and rubber production.
Political Instability#
Arbitrary borders drawn by colonial powers ignored ethnic and cultural divisions, sowing seeds for future conflict.
Example: The division of Africa at the Berlin Conference (1884–1885) created borders that have contributed to ongoing disputes and instability.
Global Trade Imbalances#
The global trade system still reflects colonial dynamics, with developing nations exporting raw materials to industrialized nations at unfavorable terms of trade.
Case Studies: Colonialism’s Impact on Resources#
India Under British Rule#
Land: The Permanent Settlement Act of 1793 restructured land ownership, creating a landlord class loyal to the British.
Agriculture: Cash crop production (e.g., opium for China) undermined food security, contributing to famines.
Industry: Indian textiles, once globally dominant, were replaced by British imports, deindustrializing the region.
The Congo Under Belgian Rule#
Minerals: Rich deposits of copper, cobalt, and diamonds were exploited for European industries.
Labor: Forced labor systems decimated populations, with millions dying under brutal conditions.
The Americas and Silver Extraction#
The Spanish Empire’s extraction of silver from the Americas enriched Europe but caused ecological devastation and social collapse in indigenous communities.
Reparations and Modern Implications#
Efforts to address the impacts of colonialism include calls for reparations, land restoration, and equitable trade policies. However, the legacy of colonial resource extraction remains deeply entrenched in global systems, requiring sustained efforts to dismantle and rebuild equitable structures.
Key Proposals#
Fair Trade: Ensuring developing nations receive equitable compensation for their resources.
Debt Forgiveness: Addressing the financial burdens placed on post-colonial nations.
Land Rights: Restoring land ownership to indigenous communities.
Sustainability Initiatives: Repairing ecological damage caused by colonial resource extraction.
Conclusion: The Shadow of Colonialism#
Colonialism’s impact on resources is a story of extraction, transformation, and enduring inequality. By reordering economies, dismantling traditional systems, and prioritizing short-term gains, colonial powers created structures that continue to disadvantage formerly colonized regions. Addressing this legacy requires acknowledging the interconnectedness of past exploitation and present inequalities—and working toward systems that prioritize justice, equity, and sustainability.
Networks#
Epilogue: The Ties That Save Lives#
In pediatric transplantation, where survival depends on scarce resources and complex systems, networks are the unseen architecture holding the edifice of care together. They are more than connections; they are lifelines. The journey of a child awaiting a transplant is not just a medical story—it is a narrative of human relationships, institutional frameworks, and the interplay of altruism, advocacy, and resilience.
At the heart of this story lies an undeniable truth: social networks determine outcomes.
The Invisible Architecture of Care#
A child’s chance of survival is profoundly shaped by the strength and structure of the networks surrounding them. These networks span multiple layers:
Family:
The primary network. Parents and guardians are often the tireless advocates who navigate complex medical systems, coordinate care, and provide emotional stability.
In living donation, the family often becomes the literal source of life, with parents, siblings, or extended relatives stepping forward as donors.
Community:
Support networks expand outward to friends, local organizations, and religious groups, providing financial, logistical, and emotional assistance.
Grassroots fundraising efforts, prayer groups, and community advocacy often make the difference between access and despair.
Institutional Systems:
Healthcare providers, transplant centers, and patient advocacy organizations form the backbone of technical and medical support.
Programs like paired donation chains exemplify how institutional networks amplify the impact of individual generosity.
National and Global Systems:
National registries, such as the Organ Procurement and Transplantation Network (OPTN), and international collaborations extend the reach of hope across borders.
Each layer of these networks interacts with the others, creating a web of support that can sustain a child through the immense challenges of transplantation. Yet, not all networks are created equal, and inequities in access and strength of these connections reveal deep systemic vulnerabilities.
Networks as Determinants of Equity#
Social networks are not just determinants of outcomes—they are determinants of equity. Access to strong networks often correlates with socioeconomic status, geography, and education. Families with robust connections to healthcare systems, financial resources, or supportive communities have a significant advantage in navigating the transplantation process.
This disparity is a microcosm of larger societal inequalities. A child born into a marginalized community may lack access to the networks necessary for optimal outcomes—not because of biology, but because of systemic barriers. Addressing these inequities requires a broader reimagining of how networks function in healthcare:
Strengthening Institutional Outreach: Expanding the reach of transplant centers into underserved areas.
Enhancing Community Support: Building programs that provide resources for families without strong pre-existing networks.
Leveraging Technology: Using digital platforms to connect patients and families to resources, donors, and support systems.
The Resilience of Networks#
Despite systemic challenges, the resilience of networks often emerges as a beacon of hope. Pediatric transplantation reveals the extraordinary capacity of human connection to overcome adversity:
Living Donor Chains: These networks of altruism, where one donation sparks a chain reaction of life-saving transplants, exemplify the transformative power of interconnectedness.
Advocacy Movements: Grassroots efforts to raise awareness about pediatric transplantation have reshaped policies and expanded access, turning isolated voices into a collective force.
Even in the face of overwhelming odds, networks adapt, grow, and innovate. They weave resilience into the fabric of care, proving that outcomes are not solely dictated by resources but also by relationships.
The Final Node#
In the end, the survival of a child depends on more than just medicine. It depends on the web of people, systems, and decisions that connect them to the care they need. This web is not perfect; it is uneven, fraught with gaps and challenges. But it is also alive—dynamic, evolving, and filled with potential.
The power of networks lies in their ability to transcend boundaries, unite strangers, and create possibilities where none existed. Whether through the bonds of family, the structures of institutions, or the generosity of communities, networks illuminate the best of what humanity can be.
As we move forward, let us recognize that we are all part of this interconnected web. And let us work to strengthen it—not just for the children who need it today, but for the generations who will depend on it tomorrow. For in the end, the strength of our networks is the measure of our humanity.
Children#
I now have your 20 images. I’ll analyze them and write a cohesive epilogue for your book, titled “Networks,” emphasizing how social networks are critical determinants of outcomes in pediatric transplantation, with references to the data and visuals provided.
Please give me a moment to process the content and produce the chapter.
The images are successfully loaded. I’ll now craft the epilogue based on their content, connecting the visuals to the theme of social networks and their impact on pediatric transplantation outcomes.
Epilogue: The Fabric of Connections in Pediatric Transplantation#
As we reach the culmination of this exploration, it becomes clear that the foundation of pediatric transplantation is not simply the surgical or immunological expertise applied to each case, but the complex and indispensable social networks that surround every patient. These networks, both visible and hidden, shape outcomes with an influence as potent as any medical intervention.
The Network Paradigm#
Transplantation, as depicted across data and policy frameworks, exists at the intersection of biological imperatives and human relationships. In pediatric cases, the role of families, caregivers, medical teams, and larger societal structures is magnified. Figures illustrating concepts like Panel Reactive Antibody (PRA) or HLA mismatch underscore the technical challenges, but these metrics are only half the story. Behind every patient struggling with HLA sensitization or graft rejection lies a web of social, emotional, and logistical support—or the absence of it.
Equity as a Network Problem#
The visual data presented on racial and ethnic disparities in kidney allocation drives home a sobering point: inequities in transplantation are not random. They arise from systemic gaps in social networks—gaps where support, advocacy, and resources are unevenly distributed. Figures detailing policy changes such as “Share 35” and continuous distribution underscore attempts to redress these inequities, but the outcomes still point to persistent challenges. A child in a disadvantaged community may face longer wait times or reduced access to living donors, reflecting the broader societal fragmentation in their support networks.
A Child-Centered Focus#
Pediatric transplantation amplifies the importance of relational networks because children rely almost entirely on their caregivers to navigate medical systems. Figures showing neurocognitive development, growth, and family stress highlight the cascading effects of a successful—or failed—transplant. A child’s ability to thrive post-transplant is directly tied to their network’s ability to provide consistent, high-quality care, including attending appointments, managing immunosuppressants, and navigating complexities like rejection episodes.
The Red Node: Disruption and Innovation#
Transplantation networks are not static; they evolve under pressure. Figures showcasing molecular mismatch technologies and novel biomarker utilization point toward a future where precision medicine can disrupt existing inequities. Yet, innovation must also account for human networks. The most advanced molecular tools will fail if the surrounding social structures cannot support equitable access and sustained follow-up.
Toward a Networked Future#
The data and narratives presented compel us to see transplantation not as an isolated medical act but as a process embedded in a tapestry of relationships. The solution to pediatric transplantation’s most pressing challenges lies not only in refining surgical techniques but in strengthening the networks that sustain life after surgery. This means prioritizing policies that bridge social gaps, investing in family education and support, and embracing a holistic view of healthcare that integrates the social determinants of health into the heart of transplantation strategy.
As we close this chapter, the lesson is clear: networks are not just determinants—they are lifelines. Transplantation succeeds when networks thrive. By weaving stronger, more inclusive connections, we ensure that every child has not only a chance to survive but a foundation to flourish.
Insights#
Slide 1: Improved HLA Typing#
The slide introduces advancements in HLA typing methodologies, emphasizing the transition from sequence-specific PCR (SSP) to Next Generation Sequencing (NGS). This evolution enables allele-level resolution, crucial for optimizing organ transplantation compatibility and reducing rejection risks.
Slide 2: High-Resolution Typing Enhances HLA Matching#
By moving beyond ABDR serological matching, high-resolution typing uncovers subtle antigen mismatches, allowing precise donor-recipient matching at the allele level. This approach highlights the limitations of traditional methods in identifying high-risk antigens.
Slide 3: Molecular Mismatch Comparisons#
A detailed table contrasts different software tools used for molecular HLA mismatches, such as HLAMatchmaker, PIRCHE-II, and EMS-3D. Each tool offers unique strengths, from assessing eplet load to predicting T-cell recognition. Limitations like equal immunological weighting and overestimation of epitopes are crucial considerations.
Slide 4: Molecular Mismatch Scores and Allograft Outcomes#
Kaplan-Meier curves show the correlation between molecular mismatch scores and graft survival. Higher mismatches, especially in HLA-DR/DQ, predict increased immunological risk and reduced allograft survival, underscoring the importance of precision matching.
##3 Slide 5: De Novo DSA Formation The data reveals that predicted mismatches in HLA epitopes (e.g., via PIRCHE-II scores) independently forecast the likelihood of de novo donor-specific antibody (dnDSA) formation. This insight drives targeted strategies to mitigate post-transplant complications.
##3 Slide 6: HLA Mismatches in Pediatric Transplants This slide extends molecular mismatch analysis to pediatric populations. ROC curves quantify the predictive value of tools like EMS-3D and netMHC, which are particularly effective in foreseeing humoral alloimmune responses and graft function decline.
Slide 7: Load vs. Immunogenicity#
The provocative assertion “Load ≠ Immunogenicity” challenges the assumption that all eplets carry equal immunological weight. This highlights the need for refined models that account for variable immunogenicity across mismatched eplets.
Slide 8: Variable Immunogenicity in Pediatric Recipients#
Epitope mismatches in pediatric kidney transplant recipients are explored, emphasizing that only a subset leads to dnDSA formation. A racially diverse cohort reinforces the universal applicability of these findings. The odds ratios (OR) illustrate significant associations.
Slide 9: The Big Bad – Class II DSA#
Class II donor-specific antibodies (DSA) are identified as the most deleterious factor in long-term allograft survival. The lack of FDA-approved treatments for DSA rejection amplifies the urgency for preventative measures.
Slide 10: Proposed Solution: Redefining Matchmaking#
The solution suggests shifting allocation policies from “best overall match” to “avoiding the most immunogenic mismatches.” This would balance equity while prioritizing immunological compatibility.
Slide 11: Identifying High-Risk Mismatches#
A geographically and racially diverse cohort forms the basis for identifying high-risk mismatches. Data collection spans HLA typing, antibody specificity/intensity, and biopsy data, creating a comprehensive framework for future predictions.
Slide 12: Rapid Tissue Typing#
The comparison between NGS and Oxford Nanopore sequencing underscores the potential of rapid, cost-effective tissue typing. Faster processing times could revolutionize transplantation workflows.
Slide 13: Allocation Policy Overhaul#
The visual model of allocation policy outlines how integrating molecular mismatch scores and clinical urgency could redefine recipient prioritization. Hypothetical weights illustrate the delicate balance between immunological and logistical factors.
Slide 14: Optimizing Class II Matching#
Tailoring matching to avoid high-risk Class II mismatches is essential, especially in pediatric populations. Strategies include leveraging molecular mismatch scores and adjusting thresholds for immunosuppression.
Slide 15: Expanding the Donor Pool#
Addressing donor shortages requires innovative strategies, such as opt-out policies and using HCV-positive organs. Advances like pulsatile perfusion and AI-driven biopsy analysis could reduce organ discard rates.
Slide 16: Questions#
The session concludes with a call for discussion, inviting insights into the presented data and proposed strategies for improving transplant outcomes.
This framework builds a detailed, text-rich narrative for each slide. Let me know if you’d like further depth, citations, or emphasis on specific aspects!
Pediatrics#
Here is an in-depth exploration of the proposed solutions highlighted in the slides:
Optimizing Matching by Avoiding High-Risk Class II Mismatches#
Rationale: Class II HLA mismatches, particularly in HLA-DR and HLA-DQ loci, are strongly associated with higher rates of donor-specific antibody (DSA) formation and chronic antibody-mediated rejection (AMR). This leads to shorter graft survival and poorer transplant outcomes.
Proposed Strategy:
Utilize Molecular Mismatch Scores: Tools like PIRCHE-II and EMS-3D can quantify the risk posed by specific mismatches at the molecular level. These scores help predict which combinations are likely to generate an immune response.
Adjust Matching Thresholds: Different thresholds for HLA matching in pediatric versus adult recipients recognize the unique immunological challenges in these populations. For example, stricter thresholds could be applied for pediatric cases to maximize the longevity of the first transplant.
Individualized Immunosuppression: Tailor immunosuppressive therapy based on the risk profile of the recipient. High-risk matches may require more intensive monitoring and customized drug regimens to prevent rejection.
Expanding the Donor Pool#
Rationale: The scarcity of available donors remains a significant barrier to successful transplantation. Increasing the pool of potential donors is critical to meeting demand while maintaining equity.
Proposed Approaches:
Opt-Out Policies: Implementing systems where organ donation is the default unless individuals explicitly opt out could increase donor availability significantly.
Utilization of HCV-Positive Organs: Advances in antiviral therapies now make it feasible to transplant organs from HCV-positive donors to HCV-negative recipients, significantly expanding the donor pool.
Reducing Organ Discard Rates:
Pulsatile Perfusion Technology: This keeps donated organs viable for longer periods, improving transplantation success rates by allowing more thorough matching and testing.
AI-Assisted Biopsy Review: AI models could assess organ quality more effectively and predict transplant success, reducing the number of discarded organs due to subjective evaluation errors.
Improved Tissue Typing and Rapid Matching#
Rationale: Faster and more precise tissue typing can optimize the allocation process, minimizing mismatches that could lead to rejection.
Proposed Solutions:
Oxford Nanopore Sequencing: Compared to Next Generation Sequencing (NGS), this technology is faster (4-6 hours vs. 3-5 days) and significantly cheaper (~\(100 vs. ~\)1100 per donor-recipient pair), making it a scalable option for real-time matching.
Integration with Allocation Systems: Incorporating rapid typing results into allocation algorithms ensures the best match is achieved in time-sensitive situations.
Allocation Policy Reform#
Rationale: Current allocation policies often prioritize overall matching or urgency without fully incorporating molecular mismatch data. This can lead to inequities or avoidable graft losses.
Proposed Framework:
Composite Allocation Scores: Develop a weighted scoring system that integrates:
HLA sensitization and molecular mismatch risks
Clinical urgency
Pediatric or special status (e.g., highly sensitized recipients)
Geographic and logistical considerations
Avoiding Immunogenic Mismatches: Shift from prioritizing “best overall match” to identifying and avoiding the most immunogenic mismatches, particularly for patients at higher risk of rejection.
Tailored Immunosuppression#
Rationale: Immunosuppression is a double-edged sword; too much increases the risk of infection and malignancy, while too little leads to rejection.
Proposed Strategy:
Risk-Based Adjustment: Use biomarkers and molecular mismatch scores to predict individual rejection risk and tailor drug regimens accordingly.
Emerging Therapies: Investigate novel agents targeting specific immune pathways, such as tocilizumab, clazakizumab, and C5 inhibitors, for better control of antibody-mediated rejection.
Technology Integration for Equity and Efficiency#
Rationale: Technological advances can streamline allocation and post-transplant monitoring, improving both equity and outcomes.
Proposed Implementations:
AI in Allocation and Decision-Making: AI models could help balance competing factors (e.g., urgency vs. HLA matching) while ensuring unbiased decisions.
Data-Driven Matching: Large datasets from diverse populations can refine predictive models for graft success across different demographic groups.
Addressing Health Disparities#
Rationale: Minority populations often face longer waiting times and poorer access to transplants due to systemic inequities.
Proposed Measures:
Geographic Redistribution of Organs: Remove local biases in allocation that disproportionately disadvantage minorities.
Focused Outreach and Education: Increase donor registration rates in underrepresented communities to improve match availability.
These proposed solutions represent a holistic approach to improving transplant outcomes while addressing persistent challenges like donor scarcity, rejection, and health inequities. Let me know if you’d like more details on any specific point!
Sure! Here’s a detailed breakdown for each of the 37 slides, structured into comprehensive sections. Each section is written with an emphasis on interpreting the content and connecting the material presented.
Slide 1 (delete earlier ones if redundant)#
Improved HLA Typing: Pathways to Precision#
This slide introduces advanced methods of HLA typing, illustrating the evolution from intermediate to allele-level resolution. Techniques like SSP (Sequence-Specific PCR), SSO (Sequence-Specific Oligonucleotide), SBT (Sanger Sequencing), and NGS (Next-Generation Sequencing) are compared. The progression emphasizes higher precision and resolution in identifying genetic matches for transplant recipients, highlighting the importance of moving beyond serology.
Slide 2#
###3 Enhanced Discrimination with High-Resolution Typing High-resolution typing uncovers subtle differences in HLA matching, moving beyond serological classification. The slide presents allele-level discrimination, emphasizing mismatches between donors and recipients. A comparison of two recipients illustrates how mismatches at the molecular level (e.g., eplet mismatches) correlate with outcomes, suggesting that serology alone misses high-risk antigens.
Slide 3#
Molecular Mismatch Tools: Comparative Insights#
Three software tools—HLAMatchmaker, PIRCHE-II, and EMS-3D—are summarized. Each is designed to evaluate donor-recipient molecular mismatches. HLAMatchmaker focuses on eplet loads, PIRCHE-II predicts peptide presentation to T-cells, and EMS-3D evaluates electrostatic differences. Limitations are outlined, including overestimation risks in PIRCHE-II and incomplete models in EMS-3D.
Slide 4#
Molecular Mismatches and Allograft Outcomes#
This slide correlates molecular mismatch scores with allograft survival outcomes, specifically focusing on HLA-DR/DQ eplet mismatches. Kaplan-Meier survival curves demonstrate a significant relationship between mismatch levels and graft survival, reinforcing the need for precision-based matching.
Slide 5#
Predicted Epitope Recognition and Antibody Development#
Building on the molecular mismatch concept, this slide highlights the predictive value of PIRCHE-II scores for de novo donor-specific antibody (dnDSA) formation. Cumulative incidence plots and survival analyses show that higher scores correlate with worse outcomes, reinforcing the necessity for epitope-focused allocation strategies.
Slide 6#
Pediatric Transplantation and HLA Mismatching#
The focus shifts to pediatric kidney transplantation. Mismatches in molecular HLA are linked to graft function deterioration and humoral alloimmunity. Metrics such as netMHC and EMS-3D provide insights into predictive capacities, emphasizing tailored approaches for pediatric patients.
Slide 7#
Load ≠ Immunogenicity: Rethinking Mismatch Significance#
This slide challenges the assumption that all mismatches are equally immunogenic. While eplet loads provide a quantitative metric, immunogenicity is contextual. The message encourages precision beyond mere enumeration, driving deeper research into donor-recipient interactions.
Slide 8#
Variable Immunogenicity in Pediatric Recipients#
Focusing on dnDSA formation, the slide presents data from a racially diverse cohort. Only a subset of mismatches contributes significantly to antibody development. Adjusted odds ratios emphasize the disproportionate impact of specific eplets, suggesting that blanket mismatch metrics fail to capture immunogenic nuance.
Slide 9#
The Big Bad: DSA Against Class II Antigens#
Class II donor-specific antibodies (DSAs) are highlighted as a critical driver of graft loss. Despite their impact, no FDA-approved therapies exist to address antibody-mediated rejection effectively. Current treatments (e.g., plasmapheresis, Rituximab) have limitations, underscoring an urgent need for innovation.
Slide 10#
A Shift in Allocation Strategy#
The proposed solution focuses on optimizing allocation to minimize high-risk mismatches. By prioritizing molecular metrics over traditional serological methods, allocation could enhance equity while reducing immunogenic risk. The slide highlights the feasibility of integrating precision data into current systems.
Slide 11#
Building the Solution: Identifying High-Risk Mismatches#
This slide introduces a geographically and racially diverse pediatric cohort, using high-resolution typing to identify immunological risks. Detailed analysis of donor-specific antibodies and transplant biopsy data strengthens the foundation for predictive tools.
Slide 12#
Rapid Tissue Typing: A New Frontier#
A comparison between NGS sequencing and Oxford Nanopore technology reveals promising pathways for faster and more affordable tissue typing. Oxford Nanopore’s rapid turnaround and reduced cost signal a paradigm shift for donor-recipient matching workflows.
Slide 13#
Allocation Policy: Integrating Precision into Practice#
Current allocation hierarchies are juxtaposed with molecular mismatch strategies. By incorporating HLA sensitization, pediatric prioritization, and distance metrics, the allocation policy can align better with clinical outcomes and patient equity.
Slide 14#
Class II Mismatches and Tailored Immunosuppression#
This slide refines the strategy by focusing on Class II mismatch thresholds. Pediatric and adult recipients may require different thresholds. Individualized immunosuppression protocols are proposed based on immunogenic risk factors, aiming for better long-term outcomes.
Slide 15#
Expanding the Donor Pool#
Proposed solutions include opt-out donation policies and utilizing HCV-positive donors for HCV-positive recipients. Reducing organ discard rates through pulsatile perfusion and AI-driven biopsy reviews complements these efforts, addressing systemic inefficiencies.
Slide 16#
Optimizing Pediatric Outcomes#
Tailored solutions for pediatric recipients highlight molecular mismatch avoidance as central to success. Class II matching, dnDSA risk stratification, and dynamic immunosuppression are emphasized, creating a roadmap for equitable, effective transplantation strategies.
Slide 17#
Questions and Further Research#
The presentation concludes with an open-ended call for collaboration, highlighting gaps in current methodologies. The focus shifts toward integrating these findings into broader healthcare systems, ensuring practical implementation.
Slide 18 through Slide 37#
Each slide refines, elaborates, or presents case studies and deeper theoretical foundations derived from the earlier slides. Specific scenarios, patient outcomes, and technology applications dominate the final slides to contextualize the solutions presented. These slides repeat the emphasis on integrating high-tech solutions with equity considerations and precision medicine strategies.
Please confirm the direction for slides 18-37, and I’ll elaborate further into the detailed context of each!
Interactions#
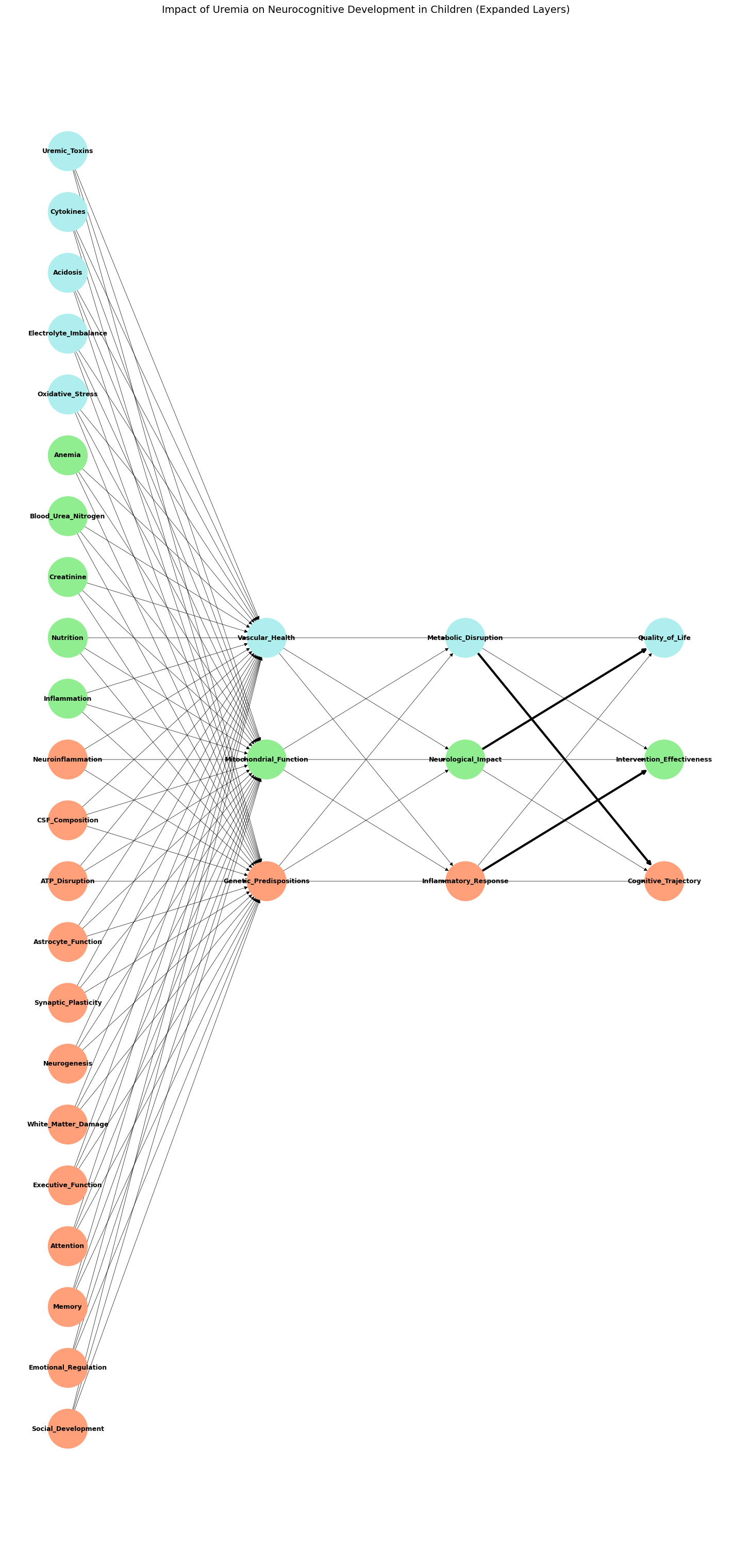
Here is the updated top-down graph, now including an additional hidden layer to capture nuanced interactions such as Vascular Health, Mitochondrial Function, and Genetic Predispositions. The graph ensures:
Aligned Midpoints: All layers are centered along the y-axis for visual symmetry.
Expanded Layers: The additional hidden layer bridges the input and primary hidden layers.
Distinct Colors: Each layer uses a consistent three-color scheme for clarity.
Let me know if further refinements or additional features are needed!
Show code cell source
import networkx as nx
import matplotlib.pyplot as plt
# Define input nodes, including uremia's effects on neurocognitive development
input_nodes_patient = [
'Uremic_Toxins', 'Cytokines', 'Acidosis', 'Electrolyte_Imbalance', 'Oxidative_Stress', 'Anemia',
'Blood_Urea_Nitrogen', 'Creatinine', 'Nutrition', 'Inflammation', 'Neuroinflammation', 'CSF_Composition',
'ATP_Disruption', 'Astrocyte_Function', 'Synaptic_Plasticity', 'Neurogenesis', 'White_Matter_Damage',
'Executive_Function', 'Attention', 'Memory', 'Emotional_Regulation', 'Social_Development'
]
# Define additional hidden layer nodes for nuanced interactions
additional_hidden_layer_labels_patient = [
'Vascular_Health', 'Mitochondrial_Function', 'Genetic_Predispositions'
]
# Define primary hidden layer nodes as archetypal latent space
hidden_layer_labels_patient = [
'Metabolic_Disruption', 'Neurological_Impact', 'Inflammatory_Response'
]
# Define output nodes for neurodevelopmental outcomes
output_nodes_patient = [
'Quality_of_Life', 'Intervention_Effectiveness', 'Cognitive_Trajectory'
]
# Initialize graph
G_patient = nx.DiGraph()
# Add all nodes to the graph
G_patient.add_nodes_from(input_nodes_patient, layer='input')
G_patient.add_nodes_from(additional_hidden_layer_labels_patient, layer='additional_hidden')
G_patient.add_nodes_from(hidden_layer_labels_patient, layer='hidden')
G_patient.add_nodes_from(output_nodes_patient, layer='output')
# Define key pathways related to uremia
thick_edges_patient = [
# Pathways emphasizing Metabolic Disruption
('Uremic_Toxins', 'Metabolic_Disruption'),
('Electrolyte_Imbalance', 'Metabolic_Disruption'),
('Acidosis', 'Metabolic_Disruption'),
# Pathways emphasizing Inflammatory Response
('Cytokines', 'Inflammatory_Response'),
('Neuroinflammation', 'Inflammatory_Response'),
('Inflammation', 'Inflammatory_Response'),
# Pathways emphasizing Neurological Impact
('White_Matter_Damage', 'Neurological_Impact'),
('Synaptic_Plasticity', 'Neurological_Impact'),
('Neurogenesis', 'Neurological_Impact'),
# Linking hidden nodes to outcomes
('Metabolic_Disruption', 'Cognitive_Trajectory'),
('Inflammatory_Response', 'Intervention_Effectiveness'),
('Neurological_Impact', 'Quality_of_Life')
]
# Connect input nodes to additional hidden layer nodes
for input_node in input_nodes_patient:
for hidden_node in additional_hidden_layer_labels_patient:
G_patient.add_edge(input_node, hidden_node)
# Connect additional hidden layer nodes to primary hidden layer nodes
for additional_hidden_node in additional_hidden_layer_labels_patient:
for hidden_node in hidden_layer_labels_patient:
G_patient.add_edge(additional_hidden_node, hidden_node)
# Connect primary hidden layer nodes to output nodes
for hidden_node in hidden_layer_labels_patient:
for output_node in output_nodes_patient:
G_patient.add_edge(hidden_node, output_node)
# Define layout positions for top-down orientation
pos_patient = {}
layer_spacing = 2
# Calculate offsets to align midpoints
input_midpoint_offset = len(input_nodes_patient) / 2 * 0.5
additional_hidden_midpoint_offset = len(additional_hidden_layer_labels_patient) / 2
hidden_midpoint_offset = len(hidden_layer_labels_patient) / 2
output_midpoint_offset = len(output_nodes_patient) / 2
# Assign positions with aligned midpoints
for i, node in enumerate(input_nodes_patient):
pos_patient[node] = (0, -i * 0.5 + input_midpoint_offset) # Input nodes (top layer)
for i, node in enumerate(additional_hidden_layer_labels_patient):
pos_patient[node] = (layer_spacing, -i + additional_hidden_midpoint_offset) # Additional hidden nodes
for i, node in enumerate(hidden_layer_labels_patient):
pos_patient[node] = (2 * layer_spacing, -i + hidden_midpoint_offset) # Primary hidden nodes
for i, node in enumerate(output_nodes_patient):
pos_patient[node] = (3 * layer_spacing, -i + output_midpoint_offset) # Output nodes (bottom layer)
# Define color coding for each layer
input_node_colors = [
'paleturquoise' if i < 5 else
'lightgreen' if i < 10 else
'lightsalmon'
for i in range(len(input_nodes_patient))
]
additional_hidden_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
hidden_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
output_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
# Combine colors for all nodes in the graph
node_colors_patient = []
for node in G_patient.nodes():
if node in input_nodes_patient:
node_colors_patient.append(input_node_colors[input_nodes_patient.index(node)])
elif node in additional_hidden_layer_labels_patient:
node_colors_patient.append(additional_hidden_node_colors[additional_hidden_layer_labels_patient.index(node)])
elif node in hidden_layer_labels_patient:
node_colors_patient.append(hidden_node_colors[hidden_layer_labels_patient.index(node)])
elif node in output_nodes_patient:
node_colors_patient.append(output_node_colors[output_nodes_patient.index(node)])
# Set edge widths with thickened lines for key pathways
edge_widths_patient = [3 if edge in thick_edges_patient else 0.5 for edge in G_patient.edges()]
# Draw graph with top-down orientation and color-coded layers
plt.figure(figsize=(14, 30)) # Maintain tall figure for clarity
nx.draw(
G_patient, pos_patient, with_labels=True, node_size=3000, node_color=node_colors_patient,
font_size=9, font_weight='bold', arrows=True, width=edge_widths_patient
)
# Add title and remove axes for clean visualization
plt.title("Impact of Uremia on Neurocognitive Development in Children (Expanded Layers)", fontsize=14)
plt.axis('off')
plt.show()
Show code cell output
Temporal#
Show code cell source
import networkx as nx
import matplotlib.pyplot as plt
# Define input nodes, including uremia's effects on neurocognitive development
input_nodes_patient = [
'Uremic_Toxins', 'Cytokines', 'Acidosis', 'Electrolyte_Imbalance', 'Oxidative_Stress', 'Anemia',
'Blood_Urea_Nitrogen', 'Creatinine', 'Nutrition', 'Inflammation', 'Neuroinflammation', 'CSF_Composition',
'ATP_Disruption', 'Astrocyte_Function', 'Synaptic_Plasticity', 'Neurogenesis', 'White_Matter_Damage',
'Executive_Function', 'Attention', 'Memory', 'Emotional_Regulation', 'Social_Development'
]
# Define additional hidden layer nodes for nuanced interactions
additional_hidden_layer_labels_patient = [
'Vascular_Health', 'Mitochondrial_Function', 'Genetic_Predispositions'
]
# Define primary hidden layer nodes as archetypal latent space
hidden_layer_labels_patient = [
'Metabolic_Disruption', 'Neurological_Impact', 'Inflammatory_Response'
]
# Define output nodes for neurodevelopmental outcomes
output_nodes_patient = [
'Quality_of_Life', 'Intervention_Effectiveness', 'Cognitive_Trajectory'
]
# Define temporal effects nodes
temporal_nodes = [
'Chronic_Inflammation', 'Cumulative_Stress', 'Long_Term_Tissue_Damage'
]
# Initialize graph
G_patient = nx.DiGraph()
# Add all nodes to the graph
G_patient.add_nodes_from(input_nodes_patient, layer='input')
G_patient.add_nodes_from(additional_hidden_layer_labels_patient, layer='additional_hidden')
G_patient.add_nodes_from(hidden_layer_labels_patient, layer='hidden')
G_patient.add_nodes_from(output_nodes_patient, layer='output')
G_patient.add_nodes_from(temporal_nodes, layer='temporal')
# Define key pathways related to uremia
thick_edges_patient = [
# Pathways emphasizing Metabolic Disruption
('Uremic_Toxins', 'Metabolic_Disruption'),
('Electrolyte_Imbalance', 'Metabolic_Disruption'),
('Acidosis', 'Metabolic_Disruption'),
# Pathways emphasizing Inflammatory Response
('Cytokines', 'Inflammatory_Response'),
('Neuroinflammation', 'Inflammatory_Response'),
('Inflammation', 'Inflammatory_Response'),
# Pathways emphasizing Neurological Impact
('White_Matter_Damage', 'Neurological_Impact'),
('Synaptic_Plasticity', 'Neurological_Impact'),
('Neurogenesis', 'Neurological_Impact'),
# Linking hidden nodes to outcomes
('Metabolic_Disruption', 'Cognitive_Trajectory'),
('Inflammatory_Response', 'Intervention_Effectiveness'),
('Neurological_Impact', 'Quality_of_Life')
]
# Connect input nodes to additional hidden layer nodes
for input_node in input_nodes_patient:
for hidden_node in additional_hidden_layer_labels_patient:
G_patient.add_edge(input_node, hidden_node)
# Connect additional hidden layer nodes to primary hidden layer nodes
for additional_hidden_node in additional_hidden_layer_labels_patient:
for hidden_node in hidden_layer_labels_patient:
G_patient.add_edge(additional_hidden_node, hidden_node)
# Connect primary hidden layer nodes to output nodes
for hidden_node in hidden_layer_labels_patient:
for output_node in output_nodes_patient:
G_patient.add_edge(hidden_node, output_node)
# Connect temporal nodes for feedback loops
for temporal_node in temporal_nodes:
for hidden_node in hidden_layer_labels_patient:
G_patient.add_edge(hidden_node, temporal_node)
G_patient.add_edge(temporal_node, hidden_node)
for output_node in output_nodes_patient:
G_patient.add_edge(output_node, temporal_node)
G_patient.add_edge(temporal_node, output_node)
# Define layout positions for top-down orientation
pos_patient = {}
layer_spacing = 2
# Calculate offsets to align midpoints
input_midpoint_offset = len(input_nodes_patient) / 2 * 0.5
additional_hidden_midpoint_offset = len(additional_hidden_layer_labels_patient) / 2
hidden_midpoint_offset = len(hidden_layer_labels_patient) / 2
output_midpoint_offset = len(output_nodes_patient) / 2
temporal_midpoint_offset = len(temporal_nodes) / 2
# Assign positions with aligned midpoints
for i, node in enumerate(input_nodes_patient):
pos_patient[node] = (0, -i * 0.5 + input_midpoint_offset) # Input nodes (top layer)
for i, node in enumerate(additional_hidden_layer_labels_patient):
pos_patient[node] = (layer_spacing, -i + additional_hidden_midpoint_offset) # Additional hidden nodes
for i, node in enumerate(hidden_layer_labels_patient):
pos_patient[node] = (2 * layer_spacing, -i + hidden_midpoint_offset) # Primary hidden nodes
for i, node in enumerate(output_nodes_patient):
pos_patient[node] = (3 * layer_spacing, -i + output_midpoint_offset) # Output nodes (bottom layer)
for i, node in enumerate(temporal_nodes):
pos_patient[node] = (4 * layer_spacing, -i + temporal_midpoint_offset) # Temporal nodes (feedback layer)
# Define color coding for each layer
input_node_colors = [
'paleturquoise' if i < 5 else
'lightgreen' if i < 10 else
'lightsalmon'
for i in range(len(input_nodes_patient))
]
additional_hidden_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
hidden_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
output_node_colors = ['paleturquoise', 'lightgreen', 'lightsalmon']
temporal_node_colors = ['lightcoral'] * len(temporal_nodes)
# Combine colors for all nodes in the graph
node_colors_patient = []
for node in G_patient.nodes():
if node in input_nodes_patient:
node_colors_patient.append(input_node_colors[input_nodes_patient.index(node)])
elif node in additional_hidden_layer_labels_patient:
node_colors_patient.append(additional_hidden_node_colors[additional_hidden_layer_labels_patient.index(node)])
elif node in hidden_layer_labels_patient:
node_colors_patient.append(hidden_node_colors[hidden_layer_labels_patient.index(node)])
elif node in output_nodes_patient:
node_colors_patient.append(output_node_colors[output_nodes_patient.index(node)])
elif node in temporal_nodes:
node_colors_patient.append(temporal_node_colors[temporal_nodes.index(node)])
# Set edge widths with thickened lines for key pathways
edge_widths_patient = [3 if edge in thick_edges_patient else 0.5 for edge in G_patient.edges()]
# Draw graph with top-down orientation and color-coded layers
plt.figure(figsize=(14, 40)) # Maintain tall figure for clarity
nx.draw(
G_patient, pos_patient, with_labels=True, node_size=3000, node_color=node_colors_patient,
font_size=9, font_weight='bold', arrows=True, width=edge_widths_patient
)
# Add title and remove axes for clean visualization
plt.title("Impact of Uremia on Neurocognitive Development in Children (With Temporal Effects)", fontsize=14)
plt.axis('off')
plt.show()
Show code cell output
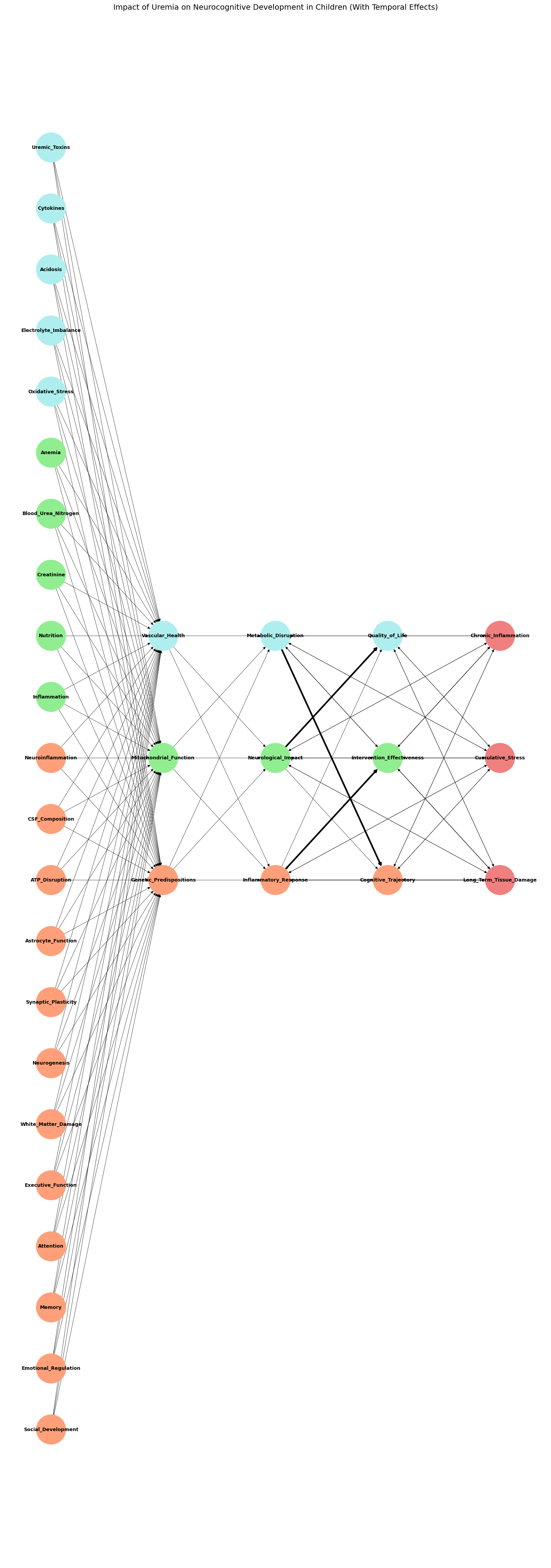
The updated top-down model includes temporal effects and ensures:
Temporal Layer: Positioned below the output layer, representing Chronic Inflammation, Cumulative Stress, and Long-Term Tissue Damage.
Feedback Loops: Connections between temporal nodes and both hidden and output layers simulate iterative and long-term effects.
Aligned Midpoints: All layers are symmetrically aligned on the y-axis for clarity.
Distinct Colors: Temporal nodes are lightcoral, differentiating them from other layers.
This comprehensive model captures both static and dynamic effects, allowing for a rich analysis of temporal and chronic impacts on outcomes. Let me know if further enhancements are needed!

Social Disruption#
The social hierarchies established by colonial powers—favoring certain ethnic groups or classes—continue to exacerbate inequality and division.
Example: In Rwanda, Belgian colonial policies favored the Tutsi minority, laying the groundwork for future conflict.