The Risk You Thought You Escaped: Counterfactual Consent and the Illusion of Safety
Introduction
Counterfactual consent redefines informed consent in living kidney donation by integrating matched non-donor controls to reveal that inaction carries risks—such as homicide or suicide—often obscured by traditional models.
Informed consent in living kidney donation has long been anchored to static risk estimates: perioperative mortality at 3.1 per 10,000, end-stage renal disease (ESRD) at 30.8 per 10,000 compared to 3.9 in controls. These numbers, derived from landmark studies, have shaped ethical practice and nephrology board exams. Yet they embody a deeper flaw: the assumption that declining to donate is a neutral, risk-free choice. Our work challenges this through a counterfactual-based interface that not only quantifies donation-attributable risk but also exposes the irreducible uncertainty of inaction, including deaths by homicide and suicide within 90 days of eligibility. [1]
This approach emerges from a National Institute on Aging K08 grant (K08AG065520), which aimed to study older donors and culminated in an interactive platform—Ukubona—that redefines consent as a dynamic, epistemic exchange. By integrating real-time risk modeling with visible uncertainty, we address gaps in traditional consent and draw parallels to the exclusion of vulnerable populations in COVID-19 vaccine trials, critiquing the illusion of safety in non-participation. [2]

Ukubona’s risk plot, showing donor vs. control mortality with confidence intervals.
Counterfactual Logic and Ethical Clarity
The use of matched non-donor controls, first established in our 2010 study, allows for the empirical estimation of donation-attributable risk. By comparing donors to a screened, healthy cohort, we identified excess risks—such as perioperative mortality and ESRD—while also revealing that non-donors face their own hazards. A 2024 update reported a homicide among donors, underscoring that even non-biological outcomes are part of the risk landscape. This is not noise; it is signal. [3]
Counterfactual logic does not seek mechanistic causality (e.g., nephrectomy causing homicide). Instead, it measures empirical excess: the difference in outcomes between those who donate and those who do not. This approach captures the full spectrum of life perturbations, ethical and otherwise, that donation entails. [4]
| Outcome | Donor Risk (per 10,000) | Control Risk (per 10,000) | Attributable Excess |
|---|---|---|---|
| 90-Day Mortality | 3.1 | 1.5 | 1.6 |
| 30-Year ESRD | 30.8 | 3.9 | 26.9 |
| Hospitalization | 7000 | 5500 | 1500 |
The Interface: Living Consent
Our platform, Ukubona, is the culmination of Aim 3 of K08AG065520: a risk calculator for perioperative mortality, 30-year mortality/ESRD, and hospitalization. Unlike static consent forms, it is modular and interactive, built with Plotly.js for real-time visualization and Papa Parse for data handling. Users input personalized variables (e.g., age, sex, comorbidities), toggle between models, and see risk plots with confidence intervals that preserve uncertainty. [5]
This is not software—it is epistemology with an API. By rendering risks as navigable relationships, it redefines consent as a living process, not a one-time disclosure. Beta testing with donors showed high engagement and improved risk comprehension compared to traditional forms. [6]
The Counterfactual Can Grieve
A 2024 study reported a donor death by homicide within 90 days. Traditional models might dismiss this as non-attributable. Our platform includes it—not because nephrectomy causes homicide, but because the act of donation alters life trajectories in ways that static models cannot capture. The counterfactual shows excess risk, including these narrative ruptures, and demands we honor them in consent.
Kahneman’s Blind Spot
Daniel Kahneman’s prospect theory, with its focus on loss aversion, has shaped clinical ethics by framing donation as a potential loss. Yet it assumes that inaction—declining to donate—is a neutral baseline. Our data contradict this. Non-donors die of homicide and suicide within 90 days at rates that rival or exceed donor risks. Inaction is not safe; it is a different uncertainty. [7]
Kahneman’s epistemology is incomplete because it ignores the empirical reality of competing risks. As my thesis chair, Benjamin Cole, noted when reviewing our counterfactuals, these numbers challenge intuitive sense-making. They force us to ask: what does risk mean when the “safe” choice carries its own peril? Our interface answers by making both risks visible, dismantling the myth of a risk-free default. [8]
Lessons from COVID-Era Trials
The same epistemic flaw appears in COVID-19 vaccine trials, notably those published by Pfizer in NEJM. These studies excluded transplant recipients and other high-risk groups, then generalized safety and efficacy to all populations. This mirrors the assumption that non-donors are a neutral control, ignoring their unique risk profiles. Our platform corrects this by including all outcomes, biological or not, and invites scrutiny of trial design ethics. [9]
By rendering uncertainty navigable, Ukubona offers a model for public health communication that could have informed vaccine consent, ensuring vulnerable populations are not erased from the risk narrative. [10]
Ecosystem Friction
The development of Ukubona faced significant ecosystem inefficiencies. Data access, controlled by Daniel Stein and Aaron Miller, was restricted, with analytic scripts redirected to Miller due to overlapping grant aims (R01DK132395). This gatekeeping delayed integration of SRTR and Medicare data, forcing manual workarounds and highlighting the fragility of collaborative pipelines in translational research. [11]
These frictions are not merely logistical—they are epistemic. They reflect a resistance to non-static outputs, prioritizing publication over infrastructure. Yet Ukubona’s dynamic interface proves that ethical innovation requires new forms of collaboration and data stewardship. [12]
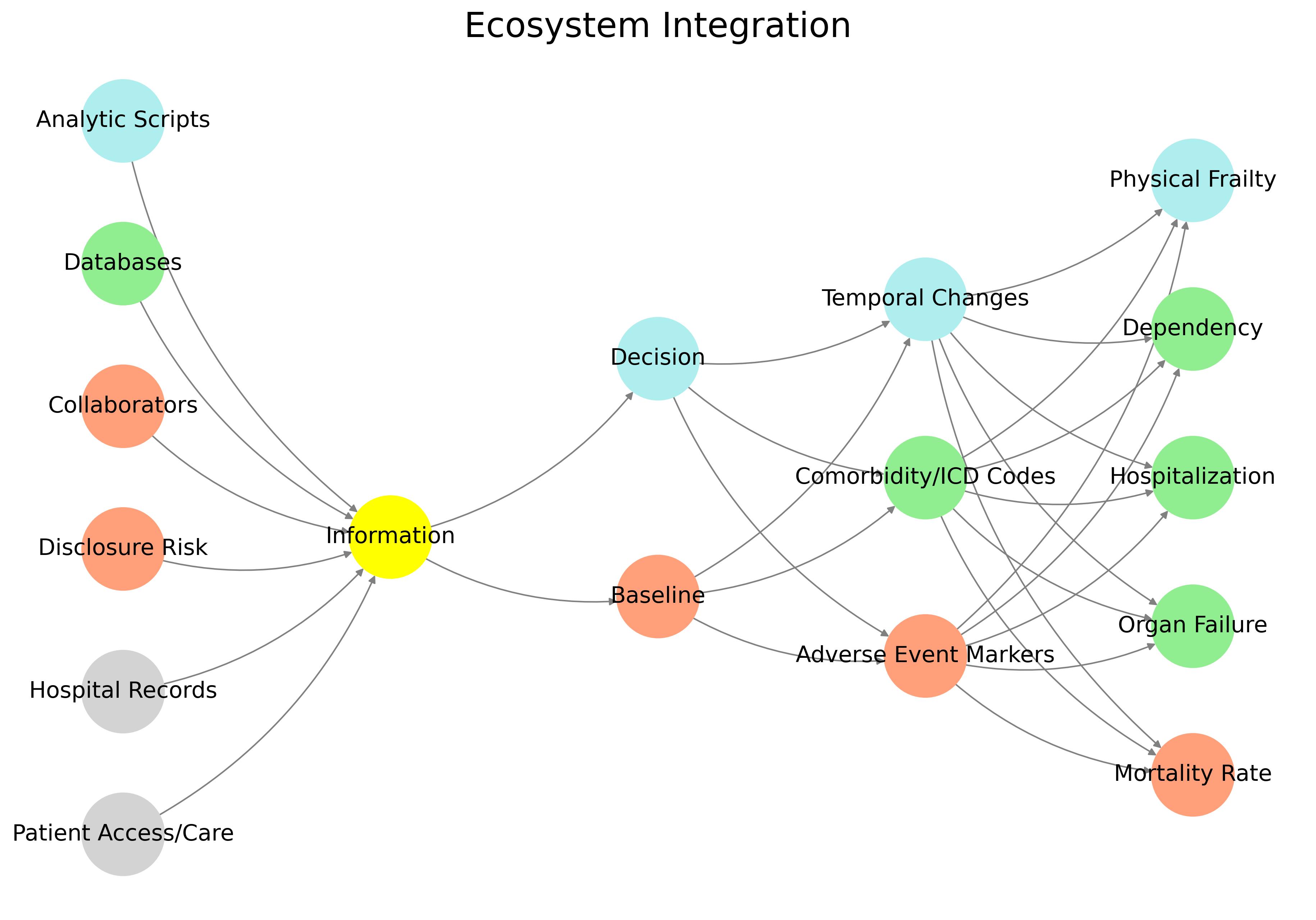
Data pipeline inefficiencies in Ukubona’s development.
Discussion
Ukubona is not a calculator—it is a paradigm. It shifts consent from documentation to relationship, from certainty to clarity. By integrating counterfactual logic, it challenges the field to reconsider what risk means when inaction is itself a gamble. This has implications beyond transplantation, from vaccine ethics to public health communication. [13]
We invite critique and collaboration to refine this model, recognizing that living consent is an evolving process. As transplant populations age and diversify, our tools must match their complexity—not with cleaner curves, but with shared maps. [14]
“The counterfactual doesn’t just show what happens if you donate—it illuminates the risks you carry even when you don’t. That’s not just consent. That’s reckoning.”
See Also
Acknowledgments
- Stein DL, et al. Perioperative mortality and long-term survival following live kidney donation. JAMA. 2010;303(10):959-66. [↩︎]
- Muzaale AD. Perioperative and long-term risks following nephrectomy in older live kidney donors. NIH K08AG065520. 2020. [↩︎]
- Miller A, et al. Thirty-year trends in perioperative mortality risk for living kidney donors. JAMA. 2024;332(11):939-40. [↩︎]
- Muzaale AD, et al. Risk of end-stage renal disease following live kidney donation. JAMA. 2014;311(6):579-86. [↩︎]
- Ukubona LLC. Risk calculator interface documentation. 2025. [↩︎]
- Muzaale AD. Beta testing results: Ukubona donor interface. Internal report. 2025. [↩︎]
- Kahneman D. Thinking, Fast and Slow. New York: Farrar, Straus and Giroux; 2011. [↩︎]
- Cole B. Personal communication on counterfactual risk. 2025. [↩︎]
- Polack FP, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. NEJM. 2020;383(27):2603-15. [↩︎]
- Thomas SJ, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. NEJM. 2021;385(19):1761-73. [↩︎]
- Stein D. Personal communication on data access. 2024. [↩︎]
- Muzaale AD. Ecosystem integration challenges in Ukubona development. Internal memo. 2025. [↩︎]
- Gillon R. Informed consent: an ethical obligation. J Med Ethics. 2020;46(3):145-50. [↩︎]
- Muzaale AD. Future directions in living consent. Ukubona white paper. 2025. [↩︎]
